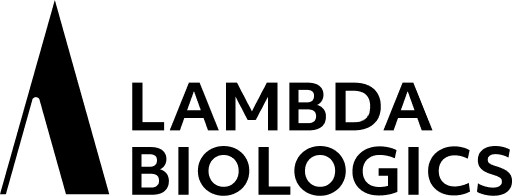
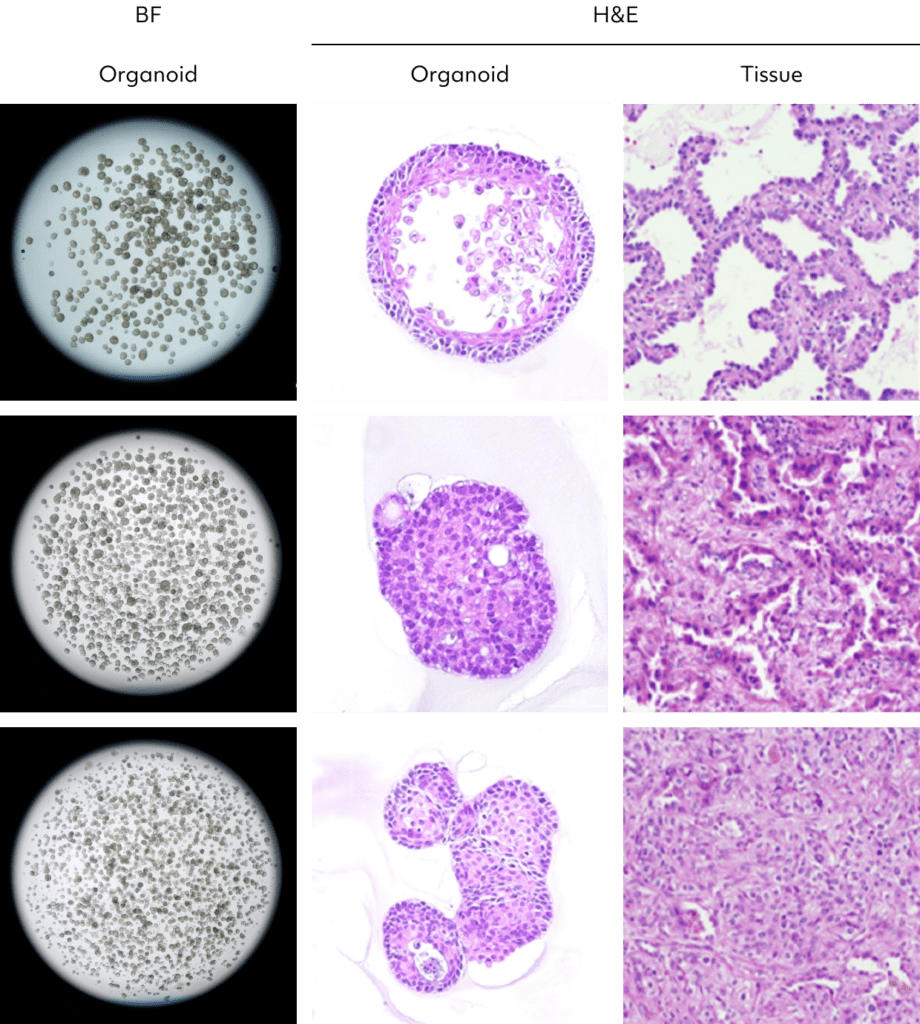
NSCLC organoids, reflecting the heterogeneity and genetic features of patient tumors, provide a versatile platform for in-depth cancer research.
These organoids faithfully mimic the tissue architecture of NSCLC, facilitating the study of tumor dynamics, invasion patterns, and drug responses.
Their patient-specific modeling capability allows personalized exploration of treatment outcomes.
NSCLC organoids contribute to understanding disease progression, identifying biomarkers, and conducting high-throughput drug screening.
In more advanced models, efforts to incorporate the tumor microenvironment enhance their relevance.
Altogether, NSCLC organoids serve as a powerful tool for advancing NSCLC biology, uncovering therapeutic strategies, and progressing toward personalized treatment approaches.
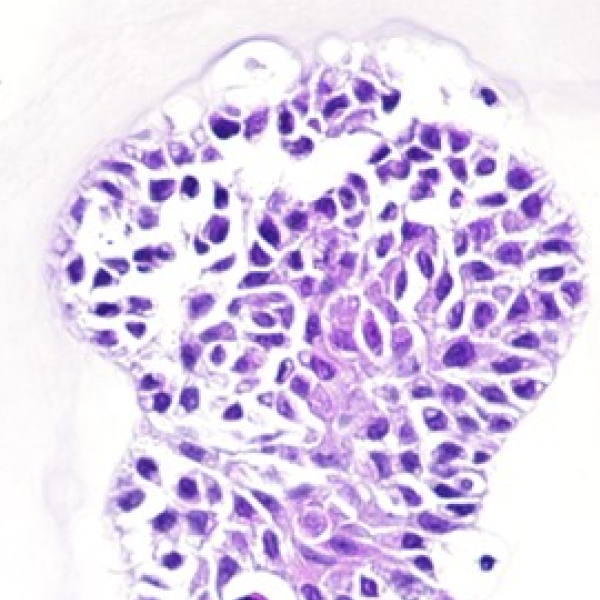
Non-small cell lung cancer organoid
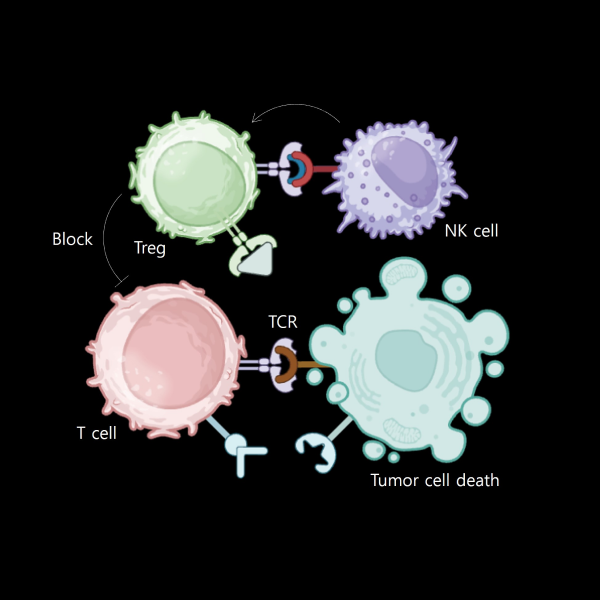
Establishing a process for isolating cytotoxic T cells that can directly attack cancer cells, creating an MHC-TCR interaction environment, and utilizing MHC I/II blockers to achieve an immune microenvironment in vivo.
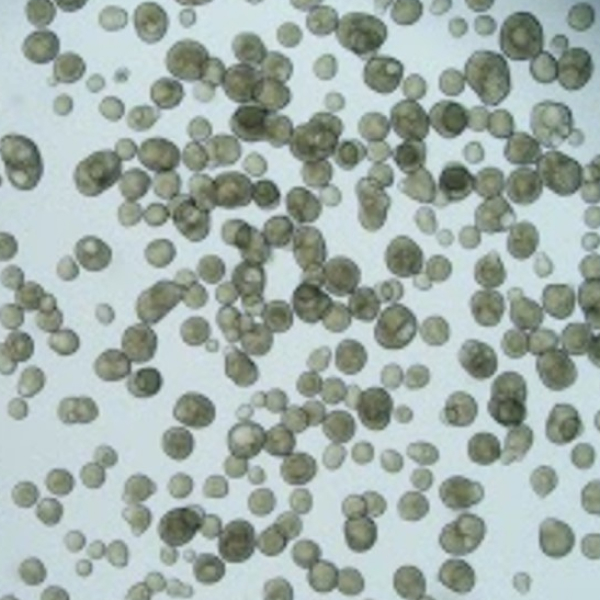
Since obtaining blood from cancer patients is limited, the process is refined by co-culturing peripheral blood mononuclear cells (PBMC) derived from healthy individuals with cancer organoids from cancer patients. This allows for the generation of cytotoxic T cells.
Regulatory T cells (Treg)” play a crucial role in maintaining immune homeostasis and tolerance by suppressing immune responses.
These lymphocytes inhibit T cell proliferation and cytokine production, thus preventing autoimmune reactions.
Our method involves evaluating the efficacy of an anticancer agent by treating a mixture of tumor organoids, cytotoxic T cells (CD8+ T cells), and regulatory T cells (Tregs) with the anticancer drug or drug candidate.
A co-culturing platform of macrophages and organoids demonstrates varying organoid cytotoxic effects depending on the ratio of M1 macrophages to M2 macrophages. Optimal cell death effects are established by co-culturing different ratios of functionally diverse immune cells. This enables the identification of optimal conditions for co-culturing various immune cells, facilitating the selection of an appropriate platform for drug testing.
Tumor-Infiltrating Lymphocytes (TILs) are predominantly found in the microenvironment of tumors, including various types of lymphocytes that have infiltrated in and around tumor tissues. Among them, CD8+ cytotoxic T cells and CD4+ helper T cells are major components. Our approach involves isolating and expanding TILs from a patient’s tumor tissue, then evaluating the efficacy of anticancer agents in a tumor microenvironment containing cancer organoids and TILs.
Preparing
NK cell
NK cells’ presence and activity in the tumor predict patient responses to treatments, linking drug efficacy to NK cell recruitment and function. NK cells actively surveil and eliminate cancer cells early on, and evaluating drug impact on NK cell-mediated immunosurveillance assesses potential in preventing tumor development. Anti-cancer drugs influence the immune microenvironment, highlighting the importance of understanding NK cell and immune milieu interplay for overall drug efficacy assessment.
Preparing
MDSC
MDSCs, create an immunosuppressive environment within tumors by inhibiting the activity of immune cells like Tcells and NK cells.
This hampers the overall anti-cancer immune response.
Moreover, MDSCs contribute to angiogenesis and metastasis, complicating the effectiveness of drugs targeting these processes.
The dual role of MDSCs as immunosuppressors and promoters of tumor-related processes poses challenges for therapies aiming to impede these crucial aspects of cancer progression.